What Is Meniere's Disease and How Is It Managed
Introduction
Meniere's disease is a chronic inner ear disorder that affects thousands of Queenslanders, causing unpredictable episodes of vertigo, fluctuating hearing loss, tinnitus, and a sensation of fullness in the ear. While the condition can be distressing and disruptive to daily life, understanding its symptoms, triggers, and management options can help you regain control and maintain your quality of life.
If you're experiencing spinning sensations, balance problems, or unexplained hearing changes, you're not alone. This comprehensive guide explores what Meniere's disease is, how it's diagnosed, and the evidence-based approaches that may help manage symptoms—from dietary modifications to medical interventions.
In This Article
- What is Meniere's Disease?
- Recognising the Symptoms of Meniere's Disease
- What Causes Meniere's Disease?
- Who Gets Meniere's Disease?
- Diagnosis Process
- Treatment and Management Options
- Lifestyle Modifications for Living with Meniere's Disease
- When to Seek Professional Help
- Professional Assessment Available on the Sunshine Coast
What is Meniere's Disease?
Meniere's disease is an inner ear disorder characterised by episodes of vertigo, fluctuating hearing loss, tinnitus (ringing in the ears), and aural fullness (a feeling of pressure or fullness in the ear). First described by French physician Prosper Menière in 1861, the condition typically affects one ear, though it can develop in both ears in approximately 15-20% of cases.
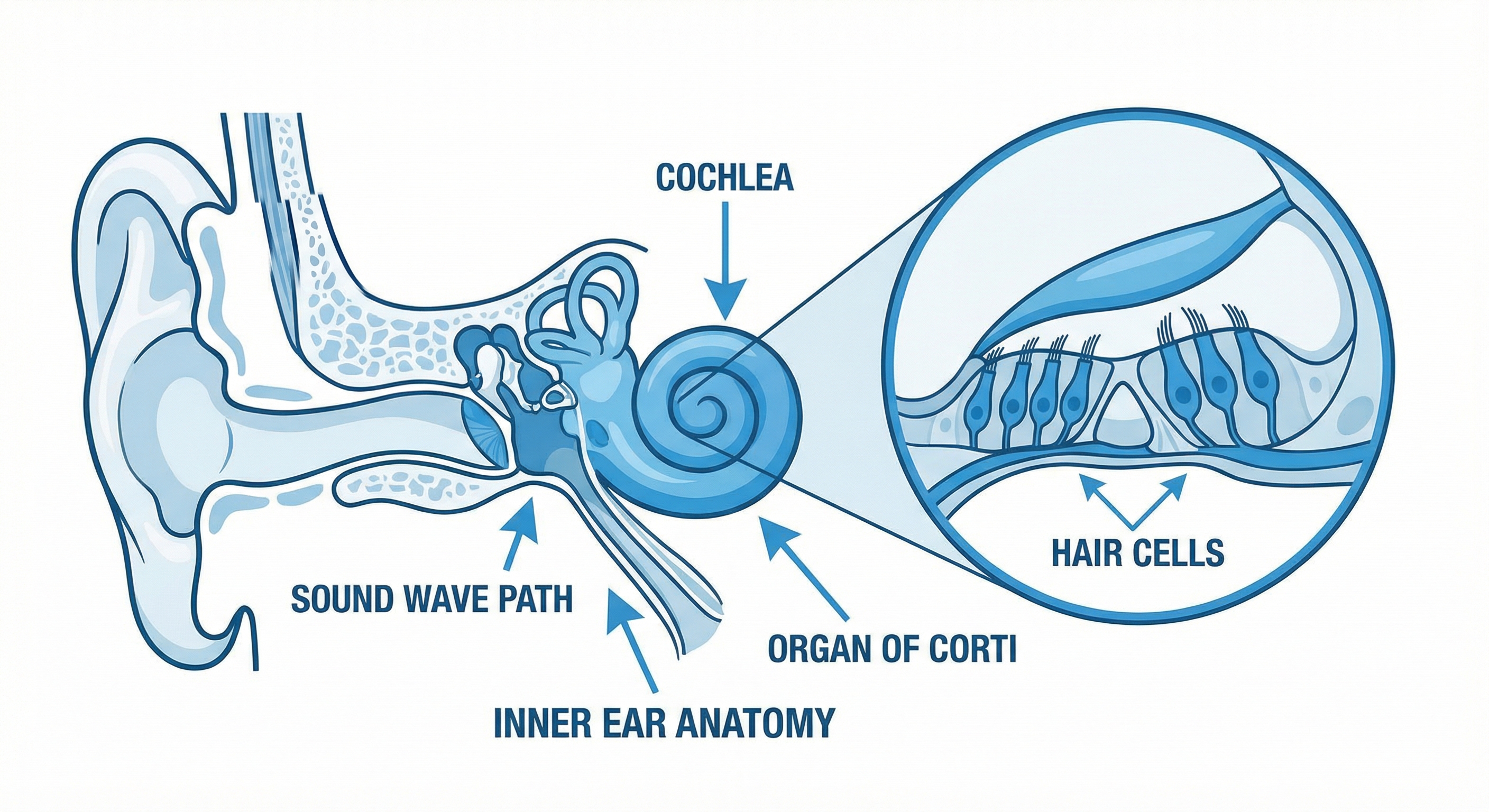
The underlying cause involves endolymphatic hydrops—an abnormal buildup of fluid (endolymph) in the inner ear's labyrinth. This fluid accumulation disrupts the normal signals your inner ear sends to your brain about balance and spatial orientation, resulting in the characteristic symptoms.
The vestibular system, which controls balance and spatial awareness, becomes compromised during Meniere's episodes. Your inner ear contains tiny structures filled with fluid that help you maintain equilibrium. When excess fluid builds up, it creates pressure that interferes with these delicate balance mechanisms.
Meniere's disease differs from other inner ear conditions because of its episodic nature—symptoms come and go, often without warning. Between episodes, many people feel completely normal, though hearing loss may progressively worsen over time.
Recognising the Symptoms of Meniere's Disease
The Classic Triad Plus Aural Fullness
Meniere's disease presents with four hallmark symptoms, often referred to as the "classic triad" plus one:
1. Vertigo and Dizziness
The most distressing symptom is typically vertigo—an intense spinning sensation that makes you feel as though you or your surroundings are rotating. These episodes:
- Last anywhere from 20 minutes to several hours
- May occur without warning
- Often force you to lie down until they pass
- Can be accompanied by nausea, vomiting, and sweating
- May leave you feeling exhausted and unsteady for hours or days afterwards
It's important to note that vertigo differs from general dizziness or lightheadedness. True vertigo creates a distinct sensation of movement or spinning.
2. Fluctuating Hearing Loss
Hearing changes in Meniere's disease have distinct characteristics:
- Usually affects low-frequency sounds initially
- Fluctuates—hearing may improve between episodes
- Gradually becomes more permanent over time
- Typically affects one ear (though both ears may be involved eventually)
- May worsen during or just before a vertigo attack
- Creates difficulty understanding speech, especially in noisy environments
Many people notice their hearing improves somewhat after an attack subsides, particularly in the early stages of the condition.
3. Tinnitus
Tinnitus associated with Meniere's disease often:
- Sounds like ringing, roaring, buzzing, or hissing
- Fluctuates in intensity, often worsening before or during attacks
- Occurs in the affected ear
- May be constant or intermittent
- Can vary in pitch and volume
The tinnitus may serve as an early warning sign that a vertigo episode is approaching.
4. Aural Fullness
This symptom is described as:
- A feeling of pressure, fullness, or blockage in the ear
- Similar to the sensation of being underwater or having your ear "clogged"
- Often present before, during, or after vertigo episodes
- May come and go between attacks
Symptom Patterns and Progression
Meniere's disease typically progresses through stages:
- Early stage: Sudden, unpredictable vertigo episodes with temporary hearing changes that recover between attacks
- Middle stage: Vertigo episodes may become less severe, but hearing loss becomes more persistent
- Late stage: Balance problems and hearing loss stabilise, but permanent hearing damage may remain; vertigo episodes may decrease in frequency or stop altogether
Not everyone follows this pattern, and progression varies significantly between individuals.
What Causes Meniere's Disease?
The exact cause of Meniere's disease remains unclear, but researchers have identified several factors that may contribute to the development of endolymphatic hydrops:
Fluid Drainage Problems
The inner ear produces endolymph fluid continuously. Normally, this fluid drains through small channels. In Meniere's disease, drainage may be blocked or inadequate, causing fluid buildup. Possible reasons include:
- Anatomical abnormalities in the endolymphatic duct or sac
- Blockages due to scarring or inflammation
- Dysfunction of fluid regulation mechanisms
Immune System Response
Some evidence suggests Meniere's disease may have an autoimmune component, where the body's immune system mistakenly attacks inner ear tissues, leading to inflammation and fluid retention.
Viral Infections
Certain viral infections affecting the inner ear may trigger or contribute to Meniere's disease development, though this connection isn't fully understood.
Genetic Factors
Meniere's disease can run in families, suggesting a genetic predisposition. However, no single gene has been identified as the cause.
Head Trauma
Previous head injuries or trauma to the ear may increase risk, particularly if they damaged inner ear structures.
Vascular Factors
Problems with blood vessel constriction or poor blood flow to the inner ear may play a role in some cases.
Environmental and Lifestyle Triggers
While not causes themselves, certain factors may trigger episodes in people who already have Meniere's disease:
- High sodium (salt) intake
- Caffeine and alcohol consumption
- Stress and anxiety
- Weather changes or barometric pressure fluctuations
- Lack of sleep
- Certain medications
- Allergies
Who Gets Meniere's Disease?
Meniere's disease can affect anyone, but certain patterns emerge:
- Age: Most commonly diagnosed in people between 40-60 years old, though it can occur at any age
- Gender: Slightly more common in women than men
- Geography: Affects people worldwide, including across Queensland's Sunshine Coast region
- Family history: Higher risk if a close family member has the condition
- Other conditions: May be more common in people with migraines, autoimmune disorders, or allergies
In Australia, Meniere's disease affects approximately 1 in 1,000 people, though mild cases may go undiagnosed. Here on the Sunshine Coast, audiologists and ENT specialists see patients regularly for diagnosis and management of this condition.
Diagnosis Process
Diagnosing Meniere's disease involves ruling out other conditions and confirming the characteristic symptom pattern. There's no single definitive test, so diagnosis relies on:
Medical History and Symptom Description
Your healthcare provider will ask detailed questions about:
- Frequency, duration, and severity of vertigo episodes
- Hearing changes and when they occur
- Tinnitus characteristics
- Sensation of ear fullness
- Other symptoms like nausea or headaches
- Family history of inner ear disorders
Hearing Tests (Audiometry)
Comprehensive hearing assessments help identify:
- Type and degree of hearing loss
- Which frequencies are affected (Meniere's typically affects low frequencies first)
- Whether hearing loss fluctuates
- Differences between ears
Balance Tests (Vestibular Function Tests)
These may include:
- Videonystagmography (VNG): Measures eye movements to assess balance function
- Vestibular evoked myogenic potentials (VEMP): Tests inner ear and vestibular nerve function
- Rotary chair testing: Evaluates how well your eyes and inner ear work together
- Posturography: Assesses which parts of your balance system you rely on most
Electrocochleography (ECoG)
This test measures electrical activity in the inner ear in response to sound, helping detect fluid buildup characteristic of endolymphatic hydrops.
Imaging Studies
While not diagnostic for Meniere's itself, MRI or CT scans may be ordered to rule out other conditions such as:
- Acoustic neuroma (benign tumour on the hearing nerve)
- Multiple sclerosis
- Structural abnormalities of the inner ear
Diagnostic Criteria
The American Academy of Otolaryngology-Head and Neck Surgery defines "definite Meniere's disease" as:
- Two or more spontaneous vertigo episodes, each lasting 20 minutes to 12 hours
- Audiometrically documented hearing loss on at least one occasion
- Fluctuating hearing loss, tinnitus, or aural fullness in the affected ear
- Not better explained by another vestibular diagnosis
Treatment and Management Options
While there's currently no cure for Meniere's disease, various treatment approaches may help manage symptoms and reduce episode frequency. Individual results vary, and professional consultation is essential to determine appropriate options.
Medications
For Acute Vertigo Episodes:
- Motion sickness medications may help reduce nausea and spinning sensations
- Anti-nausea drugs can provide relief during attacks
- Benzodiazepines may be prescribed for severe vertigo
For Long-Term Management:
- Diuretics (water pills) may help reduce fluid retention, though evidence is mixed
- Betahistine is sometimes used, though its effectiveness varies between individuals
Important: Always follow professional medical advice regarding medications. Some may cause drowsiness or interact with other drugs.
Dietary Modifications
Many people find that dietary changes help reduce episode frequency:
Sodium Reduction: Limiting salt intake to 1,500-2,000mg per day may help reduce fluid retention. Tips include:
- Reading food labels carefully
- Avoiding processed and packaged foods
- Cooking at home with fresh ingredients
- Using herbs and spices instead of salt for flavour
Caffeine and Alcohol: Some people benefit from reducing or eliminating these substances, as they may trigger episodes or worsen symptoms.
Hydration: Maintaining consistent fluid intake throughout the day (rather than drinking large amounts at once) may help stabilise inner ear fluid levels.
Trigger Foods: Keep a food diary to identify potential personal triggers such as chocolate, aged cheeses, or foods high in tyramine.
Gentamicin Injection
For severe, treatment-resistant cases, gentamicin (an antibiotic) may be injected into the middle ear. This intentionally damages the balance function of the affected ear to stop vertigo episodes. This option requires careful consideration, as it may affect hearing.
Pressure Pulse Treatment
A device called the Meniett delivers low-pressure pulses to the middle ear, which may help improve fluid exchange in the inner ear. This non-invasive option is used at home several times daily.
Vestibular Rehabilitation Therapy
This specialised physiotherapy helps your brain compensate for balance problems through:
- Eye and head movement exercises
- Balance training activities
- Gaze stabilisation techniques
- Habituation exercises to reduce dizziness responses
Surgical Options
For severe cases that don't respond to other treatments, surgical procedures may be considered:
- Endolymphatic sac decompression: Relieves pressure by draining excess fluid
- Vestibular nerve section: Cuts the balance nerve while preserving hearing
- Labyrinthectomy: Removes the balance function entirely (only when hearing is already severely damaged)
Surgery is typically reserved as a last resort after conservative treatments have been tried.
Lifestyle Modifications for Living with Meniere's Disease
Beyond medical treatment, certain lifestyle adjustments may help reduce episode frequency and improve quality of life:
Stress Management
Stress doesn't cause Meniere's disease, but many people notice stress can trigger episodes. Helpful approaches include:
- Regular relaxation practices (meditation, deep breathing, yoga)
- Adequate sleep (7-9 hours nightly)
- Time management to reduce daily pressures
- Professional counselling or support groups
Sleep Consistency
Maintaining regular sleep patterns helps overall health and may reduce Meniere's symptoms. Keep a consistent bedtime and wake time, even on weekends.
Exercise and Movement
Regular physical activity supports overall health and may improve balance function over time. Choose activities that feel safe and comfortable for your balance level. Swimming, walking, and tai chi are often well-tolerated.
Driving Precautions
Because vertigo episodes can occur suddenly, consider:
- Having someone else drive during unstable periods
- Pulling over immediately if symptoms begin while driving
- Discussing driving safety with your healthcare provider
Workplace Accommodations
If you're employed, you may benefit from:
- Flexible work arrangements during flare-ups
- A quiet workspace to reduce sensory overload
- Permission to work from home when needed
- Understanding from supervisors about unpredictable symptoms
Support Networks
Connecting with others who understand what you're experiencing can be invaluable. Consider:
- Local support groups (available in larger Sunshine Coast communities)
- Online forums and communities
- Counselling services specialising in chronic health conditions
- Family education so loved ones understand your experience
When to Seek Professional Help
Consult an audiologist or ENT specialist if you experience:
- Recurring episodes of vertigo or severe dizziness
- Hearing loss, especially if it fluctuates
- Persistent tinnitus
- Feeling of fullness or pressure in one or both ears
- Balance problems affecting daily activities
Early professional assessment is important for accurate diagnosis and appropriate management planning.
Here on the Sunshine Coast, qualified hearing healthcare professionals can provide comprehensive evaluation and coordinate care with ENT specialists when needed.
Key Takeaways
- Meniere's disease is a chronic inner ear disorder causing vertigo, fluctuating hearing loss, tinnitus, and ear fullness
- The underlying problem involves endolymphatic hydrops—excess fluid buildup in the inner ear's labyrinth
- Diagnosis requires comprehensive evaluation including hearing tests, balance assessments, and medical history
- While there's no cure, various management approaches may help reduce symptoms and episode frequency
- Dietary modifications, particularly sodium reduction, benefit many people
- Treatment options range from medications and lifestyle changes to surgical interventions for severe cases
- Individual experiences vary significantly—professional consultation is essential for personalised care
- The vestibular system and balance function are directly affected during episodes
- Stress management, consistent sleep, and identifying personal triggers may help reduce episode frequency
- Regular follow-up with qualified audiologists or ENT specialists supports effective long-term management
Professional Assessment Available on the Sunshine Coast
If you're experiencing symptoms that may indicate Meniere's disease or other inner ear disorders, comprehensive hearing and balance assessments are available throughout the Sunshine Coast region. Qualified audiologists can provide diagnostic testing, monitor hearing changes over time, and recommend appropriate management strategies tailored to your individual needs.
Early professional evaluation helps ensure accurate diagnosis and access to evidence-based management approaches. A hearing health consultation can provide clarity about your symptoms and help you explore options that may improve your quality of life.

Frequently Asked Questions
Hearing loss progression varies significantly between individuals. Some people experience minimal hearing changes, while others develop more substantial hearing loss over time. The hearing loss is typically fluctuating in early stages but may become more permanent as the condition progresses. Regular hearing assessments help monitor changes, and hearing aids may help when hearing loss affects communication.
Episode frequency varies widely. Some people have attacks daily or weekly, while others go months or even years between episodes. For many, frequency decreases over time, though hearing loss may persist. Identifying and avoiding personal triggers may help reduce episode frequency.
Stress doesn't cause Meniere's disease, but it may trigger episodes in people who already have the condition. Managing stress through relaxation techniques, adequate sleep, and lifestyle balance may help reduce episode frequency. However, stress management alone isn't sufficient treatment—professional medical care remains essential.
Meniere's disease typically begins in one ear, though approximately 15-20% of people eventually develop symptoms in both ears. This usually occurs years after initial diagnosis. Having symptoms in one ear doesn't guarantee the other ear will be affected.
Many people with Meniere's disease fly without issues, though changes in air pressure may trigger symptoms in some individuals. If you're concerned about flying, discuss precautions with your healthcare provider. It's generally advisable to avoid flying during active symptom periods.
This article is for educational purposes only. Individual results may vary. Professional hearing assessment is recommended for personalised advice.
Book Your Hearing Assessment