What Is Otosclerosis and What Are Your Treatment Options
Introduction: What is Otosclerosis?
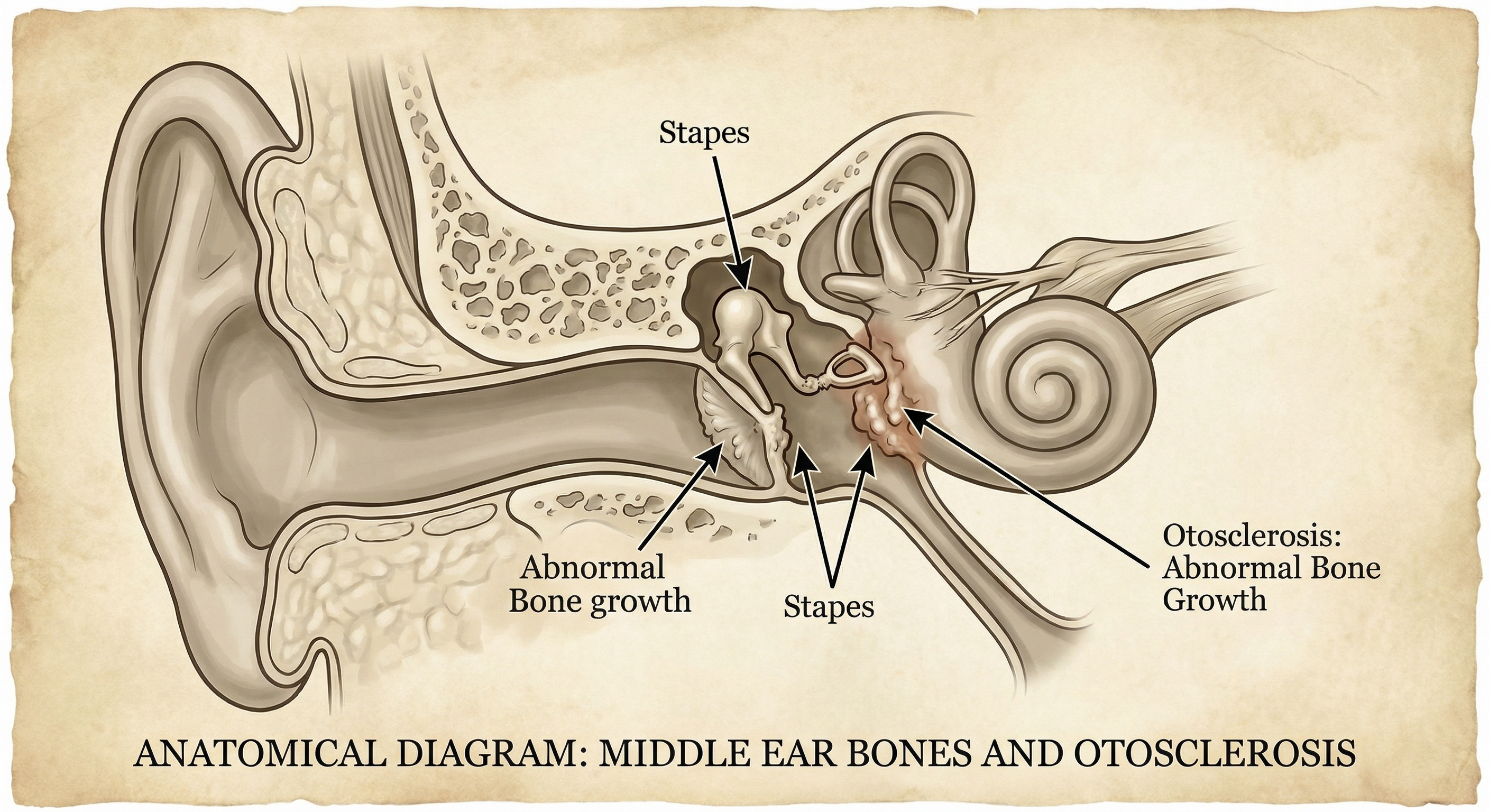
Otosclerosis is a progressive ear condition that affects the tiny bones in your middle ear, particularly the stapes bone (also called the stirrup). This condition causes abnormal bone growth that can gradually cause hearing loss over time.
The name "otosclerosis" comes from the Greek words "oto" (ear) and "sclerosis" (hardening). In this condition, normal bone in the middle ear is replaced by abnormal spongy bone growth, which eventually hardens and prevents the stapes bone from vibrating properly. This interference with normal sound transmission can lead to conductive hearing loss.
How Common is Otosclerosis?
Research suggests that otosclerosis affects approximately 0.3% to 0.4% of the general population, though many people with early-stage otosclerosis may not experience noticeable symptoms. The condition typically begins between the ages of 15 and 45, with most people noticing hearing changes in their 20s and 30s.
Women are about twice as likely as men to develop otosclerosis, and the condition appears more frequently in people of Caucasian descent. For residents of the Sunshine Coast and broader Queensland region, understanding this condition can help with early detection and timely intervention.
In This Article
How Otosclerosis Affects Your Hearing
To understand how otosclerosis impacts hearing, it helps to know how the normal hearing process works.
The Normal Hearing Process
Sound waves travel through three main sections of your ear:
1. Outer ear: Sound waves enter through the ear canal and strike the eardrum (tympanic membrane)
2. Middle ear: The eardrum vibrates and passes these vibrations through three tiny bones called ossicles (the malleus, incus, and stapes)
3. Inner ear: The stapes bone transmits vibrations to the fluid-filled cochlea, where hair cells convert them into electrical signals for your brain
This chain of events allows you to hear and interpret sounds around you.
What Goes Wrong with Otosclerosis
In otosclerosis, abnormal bone growth most commonly affects the base of the stapes bone, where it connects to the oval window (the entrance to the inner ear). This area is called the "footplate" of the stapes.
As the abnormal bone tissue develops, it can:
- Fix the stapes bone in place, preventing it from vibrating normally
- Reduce the transmission of sound vibrations to the inner ear
- Create what doctors call "conductive hearing loss" (sound can't be conducted properly through the middle ear)
In some cases, otosclerosis can also affect the inner ear structures directly, leading to sensorineural hearing loss or a combination of both types called mixed hearing loss. When otosclerosis affects the cochlea directly, this is known as cochlear otosclerosis, which can impact the delicate hair cells within the inner ear.
Symptoms and Signs of Otosclerosis
Otosclerosis typically develops gradually, and many people with otosclerosis don't notice the early signs. The most common symptom of otosclerosis is progressive hearing loss. Symptoms may vary between individuals, but common experiences include:
Primary Symptoms
Progressive hearing loss is usually the first noticeable symptom. You might find that:
- Sounds seem muffled or distant
- You need to increase the TV or radio volume more than others in your household
- You have difficulty following conversations, especially in noisy environments
- Low-pitched sounds become harder to hear initially
Tinnitus (ringing or buzzing in the ears) affects approximately 75% of people with otosclerosis. This internal sound may be constant or intermittent and can range from mild to severe.
Difficulty hearing whispered speech is often an early indicator, as soft, low-frequency sounds are typically affected first.
Additional Symptoms
Some people with otosclerosis also experience:
- Paracusis of Willis: A phenomenon where hearing actually improves in noisy environments (this occurs because background noise causes others to speak louder)
- Vertigo or dizziness: Less common, but can occur when the inner ear is affected
- Balance issues: Particularly if the condition progresses to involve the inner ear structures
Bilateral vs Unilateral Otosclerosis
Otosclerosis can affect one ear (unilateral) or it affects both ears (bilateral) in most cases:
- About 70-80% of people with otosclerosis eventually develop bilateral otosclerosis
- The condition typically starts in one ear and may progress to the other ear over months or years
- When both ears are affected, they may not progress at the same rate
- Many cases of otosclerosis begin unilaterally before becoming bilateral
Causes and Risk Factors for Otosclerosis
The exact cause of otosclerosis remains unclear, but researchers have identified several contributing risk factors for otosclerosis.
Genetic Factors
Heredity plays a significant role in otosclerosis development:
- Approximately 50-60% of people with otosclerosis have a family history of the condition
- If one parent has otosclerosis, children have about a 25% chance of developing it
- Multiple genes appear to be involved, suggesting a complex inheritance pattern
Researchers have identified specific genetic markers associated with increased risk, though genetic testing is not typically used for diagnosis.
Hormonal Influences
Hormonal factors, particularly oestrogen, appear to influence otosclerosis progression:
- Women are twice as likely to develop the condition compared to men
- Symptoms often worsen during pregnancy or after menopause
- Some women first notice symptoms during pregnancy
- Oral contraceptives have been studied as a potential risk factor, though evidence remains inconclusive
Viral Infections
Some research suggests that measles virus may play a role in triggering otosclerosis in genetically susceptible individuals. However, this connection remains under investigation, and vaccination against measles does not appear to prevent otosclerosis.
Other Potential Risk Factors
Additional factors that may contribute to or worsen otosclerosis include:
- Stress fractures in the temporal bone
- Immune system factors
- Fluoride levels in drinking water (studies have shown conflicting results)
- Ethnicity: More common in Caucasian populations, less common in Asian and African populations
How is Otosclerosis Diagnosed?
Diagnosing otosclerosis requires a comprehensive hearing assessment conducted by qualified professionals. Understanding how otosclerosis is diagnosed can help you prepare for your evaluation. Here's what you can expect during the diagnostic process:
Initial Consultation
Your audiologist or ENT specialist will:
- Review your medical history and hearing symptoms
- Ask about family history of hearing loss
- Discuss when you first noticed changes in your hearing
- Inquire about any other symptoms like tinnitus or dizziness
Otoscopic Examination
A visual examination of your ear canal and eardrum using an otoscope helps rule out other conditions that might cause hearing loss, such as:
- Ear wax buildup
- Ear infections
- Perforated eardrum
- Structural abnormalities
Audiometric Testing
Comprehensive hearing tests are essential for diagnosing otosclerosis:
Pure tone audiometry (also called an audiogram) measures your hearing sensitivity across different frequencies. With otosclerosis, this test typically shows:
- Conductive hearing loss (air conduction is reduced more than bone conduction)
- A characteristic pattern called "Carhart's notch" (a dip in bone conduction at 2000 Hz)
- Initial impact on low-frequency sounds, potentially progressing to higher frequencies
The audiogram provides a visual graph of your hearing thresholds and helps determine the type and degree of hearing loss in otosclerosis.
Tympanometry (sometimes called a tympanogram) evaluates middle and inner ear function by measuring how well your eardrum moves. In otosclerosis, the tympanogram often shows:
- Reduced eardrum mobility due to stapes fixation
- Normal ear canal volume and pressure
- A characteristic flat trace indicating stiffness in the ossicular chain
Speech audiometry assesses your ability to understand words at different volume levels, helping determine how hearing loss affects communication.
Acoustic reflex testing checks the involuntary muscle contractions in the middle ear. People with otosclerosis typically show absent or reduced acoustic reflexes.
Advanced Imaging
In some cases, your specialist may recommend:
High-resolution CT scans can reveal:
- Abnormal bone growth around the stapes footplate
- The extent of otosclerotic lesions
- Whether the cochlea is affected
MRI scans are less commonly used but can help distinguish active otosclerosis from inactive disease.
Differential Diagnosis
Your healthcare provider will rule out other conditions that can cause similar symptoms, including:
- Ossicular chain disruption
- Otitis media with effusion
- Superior semicircular canal dehiscence
- Meniere's disease
- Age-related hearing loss (presbycusis)
On the Sunshine Coast, experienced audiologists and ENT specialists use modern diagnostic equipment to accurately identify otosclerosis and develop appropriate treatment plans.
Treatment Options for Otosclerosis
Treatment for otosclerosis depends on the severity of hearing loss, how the condition affects your daily life, and your personal preferences. Understanding the available treatment options can help you make informed decisions about managing otosclerosis. The three main treatment approaches are observation, hearing aids, and surgical treatment.
Observation (Active Monitoring)
If your hearing loss is mild and doesn't significantly impact your daily activities, your healthcare provider may recommend regular monitoring without immediate intervention.
Active monitoring typically involves:
- Annual hearing tests to track progression
- Regular consultations with your audiologist
- Lifestyle adjustments to manage any hearing challenges
- Deciding on intervention if hearing loss progresses
This approach may be appropriate if you:
- Have minimal symptoms
- Can communicate effectively in most situations
- Prefer to delay other interventions
- Have medical conditions that make surgery inadvisable
Hearing Aids
Hearing aids are a non-invasive option that can effectively manage the hearing loss caused by otosclerosis. Modern hearing aid technology offers sophisticated solutions for conductive and mixed hearing loss.
How Hearing Aids Help with Otosclerosis
Hearing aids work by amplifying sound to compensate for the reduced sound transmission through the middle ear. For people with otosclerosis:
- Behind-the-ear (BTE) models are often recommended as they provide powerful amplification
- Bone conduction hearing aids may be considered for those with significant conductive loss
- Digital signal processing can target specific frequency ranges affected by the condition
- Directional microphones help with speech understanding in noisy environments
Benefits of Hearing Aids for Otosclerosis
- Non-surgical, reversible option
- Can be adjusted as hearing changes
- Suitable for people who cannot undergo or prefer to avoid surgery
- Effective for bilateral otosclerosis affecting both ears
- No recovery period or downtime
Considerations
Hearing aids are generally well-tolerated and may be the preferred long-term management strategy for many people. Professional fitting and regular follow-up appointments help ensure optimal benefit.
Stapedectomy Surgery
Stapedectomy is a surgical procedure designed to restore hearing by addressing the stapes fixation caused by otosclerosis. Otosclerosis and stapedectomy have a well-established relationship, with this microsurgical operation having been performed for decades to help many people with otosclerosis regain functional hearing.
What is Stapedectomy?
During a stapedectomy, an ENT surgeon:
1. Removes part or all of the fixed stapes bone
2. Places a prosthetic device (usually a tiny piston or wire) to restore sound transmission
3. Connects the prosthesis to the incus (another middle ear bone) and the oval window
This surgical treatment allows sound waves to properly reach the inner ear by bypassing the fixed stapes. A variation called stapedotomy involves creating a small hole in the stapes footplate rather than removing the entire bone. Many surgeons prefer this technique as it may reduce certain risks.
Surgery Considerations
Stapedectomy is typically considered when:
- Hearing loss significantly impacts quality of life
- Hearing aids are not providing adequate benefit
- The person is in good general health
- Audiometric testing confirms conductive hearing loss suitable for surgical correction
- The hearing loss in otosclerosis has progressed to a level where intervention is beneficial
What to Expect
Before surgery:
- Comprehensive hearing tests and medical evaluation
- Discussion of risks, benefits, and alternatives
- Usually performed as day surgery under local or general anaesthesia
During surgery:
- The procedure takes approximately 1-2 hours
- Performed through the ear canal without external incisions
- Requires microscopic precision and specialised instruments
After surgery:
- Most people go home the same day
- Some experience temporary dizziness or imbalance
- Hearing improvement may be noticed immediately or develop over several weeks
- Full recovery typically takes several weeks
- Follow-up appointments to monitor healing and hearing outcomes
Potential Outcomes
Research indicates that stapedectomy can be effective for many people with otosclerosis. Studies report that the success rate for stapedectomy in improving hearing ranges from 80% to 90% in experienced hands, though individual experiences vary. Your surgeon can discuss realistic expectations and success rate data based on your specific situation and their experience with the procedure.
Risks and Considerations
Like all surgical procedures, stapedectomy carries potential risks, including:
- Changes in taste sensation (temporary or permanent)
- Vertigo or balance issues (usually temporary)
- Tinnitus changes
- Rarely, injury to inner ear structures
- In some cases, hearing outcomes may not meet expectations
Your ENT surgeon will discuss these considerations in detail to help you make an informed decision.
Emerging Research and Future Treatments
Researchers continue investigating new approaches to managing otosclerosis and the treatment of otosclerosis, including:
- Medication to slow the progression of otosclerosis
- Improved surgical techniques and prosthetic devices for stapedectomy
- Regenerative medicine approaches
- Better understanding of genetic factors contributing to otosclerosis
- Investigation into ways to prevent otosclerosis in at-risk individuals
Understanding the pathophysiology of otosclerosis helps researchers develop more targeted treatment approaches for the future.
Living with Otosclerosis
Managing life with otosclerosis involves practical strategies and regular professional support. Many people with otosclerosis lead full, active lives with appropriate management.
Communication Strategies
If you're experiencing hearing loss from otosclerosis, these tips may help:
- Position yourself strategically in conversations, ensuring good lighting so you can see speakers' faces
- Reduce background noise when possible (turn off TV/radio during conversations)
- Ask others to speak clearly (not necessarily louder) and face you when talking
- Use assistive listening devices such as phone amplifiers or TV listening systems
- Inform friends, family, and colleagues about your hearing loss so they can support you
Workplace Accommodations
Many people with otosclerosis successfully manage their careers with appropriate support:
- Request seating away from noisy equipment or high-traffic areas
- Use communication technology like captioning services or amplified phones
- Arrange for written meeting notes or agenda summaries
- Consider assistive listening devices for conference rooms
Emotional Wellbeing
Hearing loss can be emotionally challenging. Some people experience:
- Frustration with communication difficulties
- Social isolation or withdrawal
- Anxiety in group situations
- Changes in self-confidence
Support resources can help:
- Connect with others experiencing hearing loss through support groups
- Discuss feelings with trusted friends, family, or counsellors
- Focus on effective management strategies rather than limitations
- Maintain social connections and activities you enjoy
Regular Monitoring
Whether you choose observation, hearing aids, or surgery, ongoing professional support is important:
- Annual hearing assessments to track any changes
- Regular hearing aid maintenance and adjustments if applicable
- Follow-up with your ENT surgeon if you've had stapedectomy
- Prompt consultation if you notice sudden hearing changes or new symptoms
Pregnancy Considerations
Women with otosclerosis who are planning pregnancy should discuss their situation with healthcare providers, as:
- Some women experience progression during pregnancy
- Hormonal changes may affect symptoms
- Treatment timing might need consideration around pregnancy plans
Key Takeaways
- Otosclerosis is a progressive ear condition involving abnormal bone growth in the middle ear that can cause hearing loss, typically beginning between ages 15-45
- Genetics play a significant role, with about 50-60% of affected individuals having a family history of the condition
- Symptoms usually develop gradually, starting with low-frequency hearing loss, possible tinnitus, and difficulty hearing in certain situations
- Comprehensive diagnostic testing by an audiologist or ENT specialist is essential for accurate diagnosis and treatment planning
- Three main management approaches exist: observation with monitoring, hearing aids, and stapedectomy surgery
- Hearing aids are effective non-surgical options that can successfully manage otosclerosis-related hearing loss for many people
- Stapedectomy may be considered when hearing loss significantly impacts quality of life and other factors support surgical intervention
- Regular professional monitoring helps track progression and ensures your management strategy continues meeting your needs
- Communication strategies and support can help you manage daily activities and maintain quality of life with otosclerosis
Next Steps
If you're experiencing progressive hearing loss, tinnitus, or other symptoms that concern you, professional assessment is the first step toward understanding your hearing health.
At Hearing Care on the Sunshine Coast, our experienced audiologists provide comprehensive hearing evaluations using modern diagnostic equipment. We can help determine whether otosclerosis or another condition may be affecting your hearing and discuss management options appropriate for your situation.
Contact us to arrange a hearing assessment at your convenience. Individual results and experiences vary, and personalised professional advice is essential for optimal hearing health outcomes.

Frequently Asked Questions
No, otosclerosis and age-related hearing loss (presbycusis) are different conditions. Otosclerosis involves abnormal bone growth affecting the middle ear bones and typically begins earlier in life (20s-40s). Age-related hearing loss usually starts after age 50 and primarily affects the inner ear. The two conditions have different causes and may require different management approaches, though both can sometimes occur in the same person.
Hearing aids can be very effective for managing hearing loss caused by otosclerosis. Many people successfully use hearing aids long-term without surgery. Hearing aids are particularly effective for the conductive component of hearing loss in otosclerosis. The choice between hearing aids and surgery depends on multiple factors including the degree of hearing loss, your lifestyle needs, overall health, and personal preferences. Both options can be appropriate, and some people choose hearing aids first and consider surgery later if needed.
If you have bilateral otosclerosis (affecting both ears), you might eventually benefit from surgery in both ears. However, surgery is typically performed on one ear at a time, with several months between procedures if both ears require treatment. Some people find that having surgery in one ear provides sufficient hearing improvement for their needs. Your ENT surgeon can help determine the best approach based on your hearing in each ear.
Untreated otosclerosis rarely leads to complete deafness, but it can cause significant hearing loss over time. In most cases, the conductive hearing loss (related to middle ear bone fixation) can potentially be addressed with hearing aids or surgery. When otosclerosis affects the inner ear structures (causing sensorineural hearing loss), more advanced management may be needed. Regular monitoring and timely intervention help maintain functional hearing for most people with the condition.
Otosclerosis is not classified as an autoimmune disease. While researchers continue studying the cause of otosclerosis, current evidence suggests it involves abnormal bone remodeling in the middle ear rather than an autoimmune process. However, some studies have investigated potential immune system involvement in the progression of otosclerosis. The condition appears to have strong genetic factors and may be influenced by hormonal changes, but it doesn't meet the criteria for autoimmune diseases.
The prognosis for otosclerosis varies depending on individual circumstances and chosen treatment approaches. With appropriate management through hearing aids or surgical treatment, many patients with otosclerosis maintain good functional hearing throughout their lives. The progression of otosclerosis differs between individuals—some experience slow, gradual hearing changes while others may notice more rapid progression. Regular monitoring by an audiologist helps track the progression of otosclerosis and adjust treatment strategies as needed. Early diagnosis and treatment generally lead to better outcomes for managing hearing loss in otosclerosis. --- ## How is Otosclerosis Treated? Otosclerosis is treated through one of three main approaches depending on severity and individual circumstances. Some patients with otosclerosis may benefit from observation and monitoring, while others find that hearing aids effectively manage their symptoms. For those seeking a more permanent solution, stapedectomy surgery offers the potential to restore hearing by addressing the underlying cause of otosclerosis. The best treatment for otosclerosis depends on factors including the degree of hearing loss, how otosclerosis affects daily life, and personal health considerations.
This article is for educational purposes only. Individual results may vary. Professional hearing assessment is recommended for personalised advice.
Book Your Hearing Assessment